Vulvodynia: Symptoms, Causes, and Treatment Options for Chronic Vulvar Pain
SexForEveryBody.com is supported by our readers. We may earn a commission if you buy through links on our site. Learn more.

Frequently unavoidable and not often discussed, chronic genital pain is a reality for millions of Americans.
For people with vaginas, vulvar pain, in particular, is both prevalent and misunderstood.
I’m familiar with the confusion surrounding persistent vulvar pain because I experienced it for three years without a diagnosis. During that time, I scoured the Internet for clues about what might be causing my discomfort, largely to no avail.
Finally, after a year of intensive visits to gynecologists and various specialists, I was eventually diagnosed with vulvodynia.
What is vulvodynia?
Vulvodynia is defined as chronic pain of any kind around the opening of the vagina that does not have an identifiable cause and lasts for at least three months. The condition affects roughly 16% of people who have vaginas in the U.S. at some point in their lives.
Vulvodynia can be diagnosed more specifically based on the location and cause of pain. A diagnosis of either localized or generalized vulvodynia will be made depending on where the discomfort occurs in the vulva.
There are different types of vulvodynia, including localized and generalized
Localized vulvodynia is pain that is confined to one area of the vulva. There are two predominant locations for localized vulvodynia: the clitoris and also the vestibule, which is the tissue surrounding the vaginal opening.
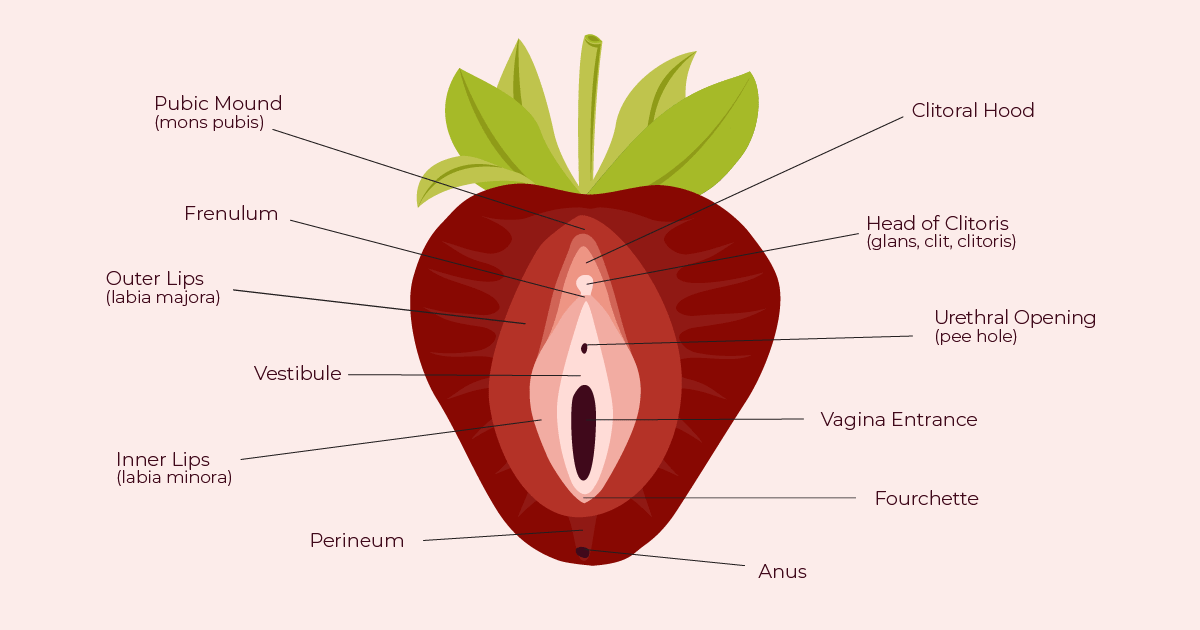
Vestibulodynia, formerly known as vulvar vestibulitis syndrome (VVS), causes pain in the area around the vaginal opening called the vestibule. This form of vulvar pain does not include the clitoris or the anus.
The most common form of vestibulodynia is called provoked vestibulodynia (PVD) and is diagnosed when pain occurs during or after pressure is applied to the vestibule.
There are two types of PVD, referred to in the medical community as either primary or secondary.
Primary PVD is when vestibular pain occurs upon the first attempt of vaginal penetration. On the other hand, a diagnosis of secondary PVD is made when pain-free intercourse was possible before the development of vestibular pain.
Generalized vulvodynia, on the other hand, is characterized by pain that occurs spontaneously and somewhat constantly on various parts of the vulva. The pain is often described as a persistent burning in the vulva.
What causes vulvodynia?
Doctors are unsure about the direct causes of vulvodynia. Research shows that there are many possible contributing factors, including nerve damage, allergies, hormonal changes, muscle spasms in the pelvic floor, and a history of vaginal infections.
How is vulvodynia diagnosed?
Unlike diseases or infections that can be detected using lab tests, vulvodynia can only be diagnosed through a process of elimination.
To reach the proper diagnosis, your healthcare provider should ask questions about your medical, surgical, and sexual history and may take swabs and perform a pelvic health exam to rule out other possible causes.
Once a diagnosis has been made, it is important to work closely with your healthcare provider to find the best treatment option for you.
What is the best treatment for vulvodynia?
There is no established cure for vulvodynia because its causes and effects vary so widely from one person to the next. Finding the right treatment option may be a long process because of the difficulty of locating the cause of the condition. However, having the best combination of treatments can greatly reduce vulvar pain symptoms.
Possible vulvodynia treatments include medication, biofeedback therapy, local anesthetics, nerve blocks, pelvic floor physical therapy, and, in rare cases, surgery.
Your healthcare professional may also recommend counseling, as vulvodynia is linked to a higher rate of depression and sexual dysfunction. Seeing a counselor can help people learn how to cope or manage vulvodynia symptoms and increase their overall quality of life.
Home remedies for vulvar pain
Some people find that adding home remedies to their treatment plans helps further alleviate symptoms. For vulvar pain management, doctors recommend cold compresses or gel packs. Using lubrication during sexual activity can also help reduce irritation.
Taking a sitz bath can also temporarily reduce vulvodynia symptoms. A sitz bath is a shallow, warm bath that cleans and can soothe the perineum, which is the area between the vulva and the anus. Although it is possible to give yourself a sitz bath in a bathtub, you can also buy a sitz bath kit that fits over the toilet.
To prevent flare-ups of vulvar pain, it is best to avoid tightfitting underwear and pantyhose, hot tubs and soaking in hot baths, scented tampons or pads, and activities that put pressure on the vulva.
Relief is possible
Again, there is no one “cure” for vulvodynia. However, with the right treatment plan, it is possible to experience relief from vulvodynia symptoms.
If you want to learn more about my journey from chronic vulvar pain to diagnosis and eventually to pain relief, read my article at FutureofSex.net “Vulvodynia: My 3-Year Journey to Diagnosis and Relief from Chronic Genital Pain.”
This article is for informational purposes only and is not intended to replace medical advice from a licensed physician or other health professionals.
Image sources: Timothy Meinberg, Alex B. Porter
Keats Iwanaga is a passionate writer and reader who strives to use her voice to uplift marginalized communities through writing and volunteer work. This is a focus of the articles she writes for FutueofSex.net and SexforEveryBody.com.
She authors stories with a focus on destigmatizing discussions of sexual health and wellness. A passionate volunteer, she serves as an administrative assistant at a local LGBTQ+ counseling center.
Keats graduated from the University of California, Berkeley in 2019 with a BA in Art History and a minor in Race and Law. She was awarded High Distinction in General Scholarship and from the Art History department.